Minimizing the Impact of Antimicrobial Resistance
A Summary of the 2020-2025 CDC National Action Plan for Combating Antibiotic-Resistant Bacteria.
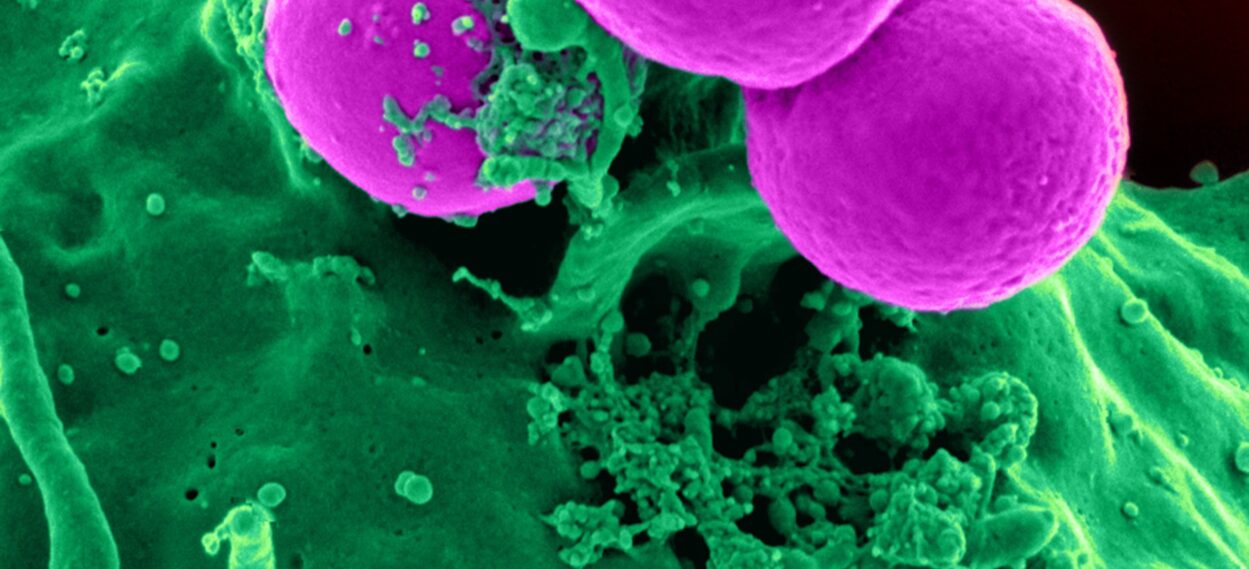
Health and life expectancy in the US have improved due to the reduction in deaths caused by bacterial infections achieved through discovery and development of antibiotics, improved hygiene and sanitation, and vaccinations. However, the emergence and spread of antibiotic resistance presents challenges to current infection prevention and treatment strategies. According to the CDC, it is estimated that antibiotic-resistant organisms cause over 2.8 million infections and nearly 36,000 deaths each year and are associated with billions of dollars in healthcare costs annually. Targeted actions to prevent the spread of antibiotic-resistant infections and preserve effectiveness of antibiotics are needed to help improve these statistics.
Based on the need for strategies to improve response to antibiotic resistance threats, the Federal Task Force for Combating Antibiotic-Resistant Bacteria (CARB) established their first National Action Plan in 2015. They have recently updated this report and built upon its ideas in their 2020-2025 National Action Plan for CARB, which maintains five goals for reducing antibiotic-resistant infections established in the National Strategy shown below:
Source: National Action Plan for Combating Antibiotic-Resistant Bacteria
The goals above focus on improving appropriate antibiotic use and antimicrobial development as well as improving infection prevention and control through antibiotic resistance detection and surveillance.
The 2020 Plan includes new objectives and targets to help achieve the five established goals and measure progress towards their achievement. The goals and challenges anticipated relating to their achievement as outlined in the 2020 Plan are summarized below.
Goal 1: Slow the Emergence of Resistant Bacteria and Prevent the Spread of Resistant Infections
Primary prevention of antibiotic-resistant infections is a key method of reducing the impact these infections have on human and animal health. Spread of infections can be prevented through infection control and biosecurity measures, including improvement of antibiotic resistance detection and monitoring and containment of outbreaks. Antibiotic resistance can be delayed or prevented through judicious use of antimicrobials. Reducing antibiotic overuse can also help prevent antibiotic-related adverse events and secondary infections, including Clostridioides difficile infections. Improvement in antibiotic use can be accomplished through antibiotic stewardship initiatives, not only in humans, but also in animal health and crop protection communities. Challenges related to this goal include difficulties in accomplishing behavior changes and buy-in amongst prescribers and other stakeholders, as well as identifying best practices in infection control and ensuring they are implemented across all areas of healthcare.
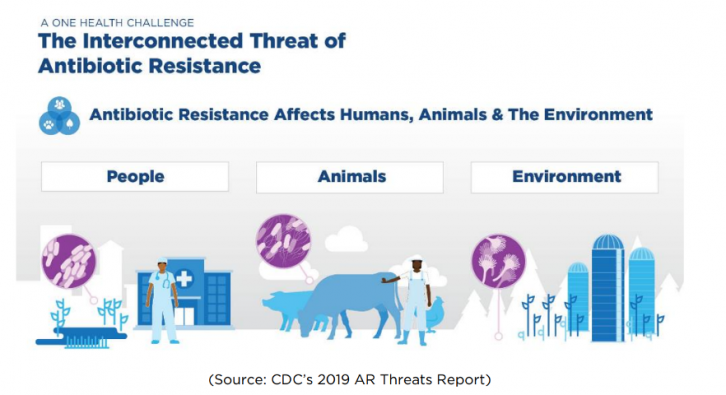
Goal 2: Strengthen National One Health Surveillance Efforts to Combat Resistance
The concept of One Health calls for recognition that many health issues in humans are closely related to health issues in animals and the environment as well. Antimicrobial resistance is considered a One Health issue per the CDC, meaning that efforts targeted at identifying, monitoring, and managing effects of antibiotic-resistant organisms as well as antibiotic use and misuse must encompass human, animal, and plant populations in order to be effective. Measures aimed at enhancing testing capabilities for whole-genome sequencing and resistance testing, as well as expanding research repositories and resistance databases, will allow improved surveillance of antibiotic resistance. Challenges related to this goal include difficulties with data collection and sharing amongst partners in all sectors of One Health, availability of lab personnel, training, and resources, and effective, timely, and consistent electronic reporting and surveillance.
Goal 3: Advance Development and Use of Rapid and Innovative Diagnostic Tests for Identification and Characterization of Resistant Bacteria
Effective treatment and control of infections caused by antibiotic-resistant organisms requires prompt identification, which can be accomplished through appropriate implementation of new diagnostics into clinical and veterinary care, including point-of-care resistance testing for outpatient clinical settings. As new diagnostics are developed, research and training relating to result interpretation and application to clinical practice are necessary in order to best guide the use of these tools to improve antibiotic use and clinical outcomes. Expanding use of existing diagnostic tools will also improve identification and management of antibiotic-resistant infections. Challenges related to this goal include high costs associated with test components, reagents, and labor and training associated with implementation. Research relating to best practices for use is also necessary, which presents an additional barrier to timely implementation of new technologies.
Goal 4: Accelerate Basic and Applied Research and Development for New Antibiotics, Other Therapeutics, and Vaccines
As antibiotic resistance continues to emerge, innovations in antimicrobial therapy are necessary to combat infections caused by antibiotic-resistant organisms. Research into the development and spread of antimicrobial resistance can improve understanding and provide a basis for development of new treatment and prevention strategies. These include new antibiotics, other therapeutics (including bacteriophages, immune modulators, and monoclonal antibodies), and vaccines. Challenges related to this goal include the time and resources required for discovery of new therapeutic targets within resistant bacteria as well as development of new therapeutics and vaccines with acceptable safety and efficacy characteristics.
Goal 5: Improve International Collaboration and Capacities for Antibiotic-Resistance Prevention, Surveillance, Control and Antibiotic Research and Development
The US Government works in collaboration with local, national, and international communities to address antibiotic resistance development and spread through rapid detection and biocontainment strategies. Concerted research and resource allocation efforts would allow for enhanced evaluation of new and existing therapeutics and management strategies and promote development of new and improved diagnostics, therapeutics, vaccines, and infection control practices. It would also improve understanding of antibiotic resistance development and spread and allow for the generation of more effective mitigation strategies. Challenges related to this goal include achievement of global consensus surrounding practice guidance and recommendations, the necessity of supporting resistance identification, prevention, and management efforts in partnering countries, and the establishment of an international network capable of responding to antibiotic resistance in a concerted manner with regards to resource allocation.
Planned annual reports will announce progress toward these goals and new or updated targets. For more information on the CDC National Action Plan for CARB, visit https://www.cdc.gov/drugresistance/
us-activities/national-action-plan.html.

This content was provided by Molly Miller, Infectious Diseases Pharmacist with Nebraska Medicine.


