Outpatient Antibiotic Stewardship Assessment Tool

Due to the increasing threat of antibiotic resistance, antibiotic stewardship is a vital function within healthcare systems to ensure that antibiotics are being used appropriately. The Centers for Disease Control and Prevention (CDC) defines antibiotic stewardship as “the effort to measure antibiotic prescribing; to improve antibiotic prescribing by clinicians and use by patients so that antibiotics are only prescribed and used when needed; to minimize misdiagnoses or delayed diagnoses leading to underuse of antibiotics; and to ensure that the right drug, dose, and duration are selected when an antibiotic is needed.” While stewardship is often associated with acute care hospitals or long-term care facilities, it is arguably even more important in outpatient settings because of the volume of patients passing through these areas, with approximately 60% of antibiotic use in the United States related to care received in outpatient settings.
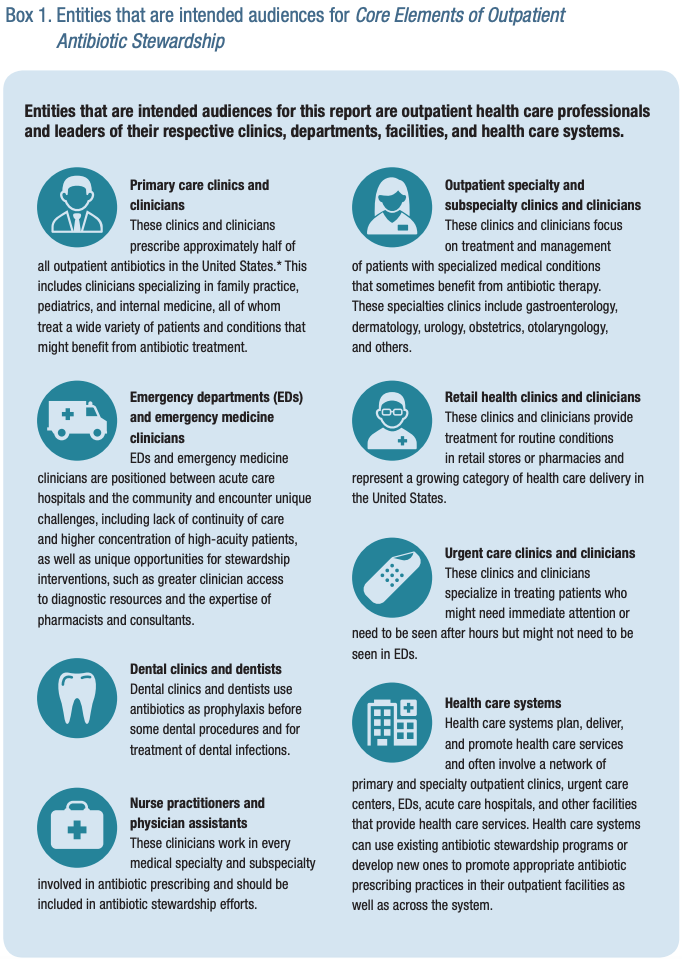
To assist in the development of antibiotic stewardship practices in outpatient facilities, the CDC released the report, Core Elements of Outpatient Antibiotic Stewardship. This report provides helpful resources and guidance to all entities interested in improving outpatient antibiotic prescribing and use, including clinicians (e.g., physicians, dentists, nurse practitioners, and physician assistants) and clinic leaders in primary care, medical and surgical specialties, emergency departments, retail health and urgent care settings, and dentistry, as well as community pharmacists, other health care professionals, hospital clinics, outpatient facilities, and health care systems involved in outpatient care.
Source: https://www.cdc.gov/antibiotic-use/community/pdfs/16_268900-A_CoreElementsOutpatient_508.pdf
In this document, the CDC establishes 4 Core Elements of outpatient antibiotic stewardship: commitment, action for policy and practice, tracking and reporting, and education and expertise.
Commitment represents all health care team members striving for appropriate use of antibiotics, from administration to frontline staff. This includes creating (and displaying) policies or written commitments supporting antibiotic stewardship, identifying a leader to direct stewardship activities, and communicating with staff about antibiotic stewardship efforts.
Action for policy and practice includes the creation and implementation of policies and interventions to improve antibiotic use. Some examples of these include providing evidence-based treatment guidelines for clinicians, implementing clinical decision support to improve antibiotic prescribing, or encouraging watchful waiting without antibiotic prescription when appropriate (e.g., acute uncomplicated sinusitis, mild acute otitis media).
Tracking and reporting is a very important core element that can be used to improve antibiotic use over time. This tracking can occur at the facility level, but it is most helpful when done at the individual prescriber level. Once data is tracked, it is important to act on it to help improve use through individualized feedback and continuous quality improvement processes.
Education and expertise are vital to improving antibiotic use and should target both patients and clinicians. Education for patients and families can help improve health literacy, guide patients on symptomatic relief in conditions that do not require antibiotics, and reinforce when antibiotics are and are not needed. Clinician-targeted education can focus on appropriate indications for antibiotics and communication strategies for tempering patient expectations regarding antibiotics, among others.

Source: https://www.cdc.gov/antibiotic-use/community/pdfs/16_268900-A_CoreElementsOutpatient_508.pdf
Implementing these 4 Core Elements is a process that takes dedicated time and resources but provides large benefits to individual clinics as well as the healthcare system as a whole. To help assist facilities, Nebraska ASAP has created a self-assessment tool to be used by clinics and other outpatient facilities. This tool can help facilities identify areas that still need work as well as any potential barriers. This resource is available below as well as on the Tools and Templates tab for Ambulatory Care, and we plan to create an online survey-based version in the near future. For any questions about the assessment tool, interpretation of results, or next steps that can be taken after completing the assessment, feel free to reach out to Nebraska ASAP at anwatkins@nebraskamed.com.
Antimicrobial Stewardship Self-Assessment Instrument for Outpatient Facilities
 This content was provided by Andrew B. Watkins, Pharmacy Coordinator of Nebraska ASAP. Feel free to send any questions to anwatkins@nebraskamed.com.
This content was provided by Andrew B. Watkins, Pharmacy Coordinator of Nebraska ASAP. Feel free to send any questions to anwatkins@nebraskamed.com.

