The State of Antimicrobial Stewardship In the U.S. and Nebraska

Antimicrobial stewardship is the coordinated efforts to prescribe antimicrobial appropriately and consume antimicrobial responsibly in order to maximize clinical outcomes while minimizing unintended consequences of antimicrobial use. In recent years, major emphasis from the human and animal health sectors as well as public health and regulatory agencies has been placed on the implementation of antimicrobial stewardship efforts to improve antimicrobial use. The emphasis in this area has led to the increased availability of antimicrobial stewardship resources (such as the Nebraska ASAP) and the increased awareness that antimicrobials are important life-saving resources that need to be preserved.
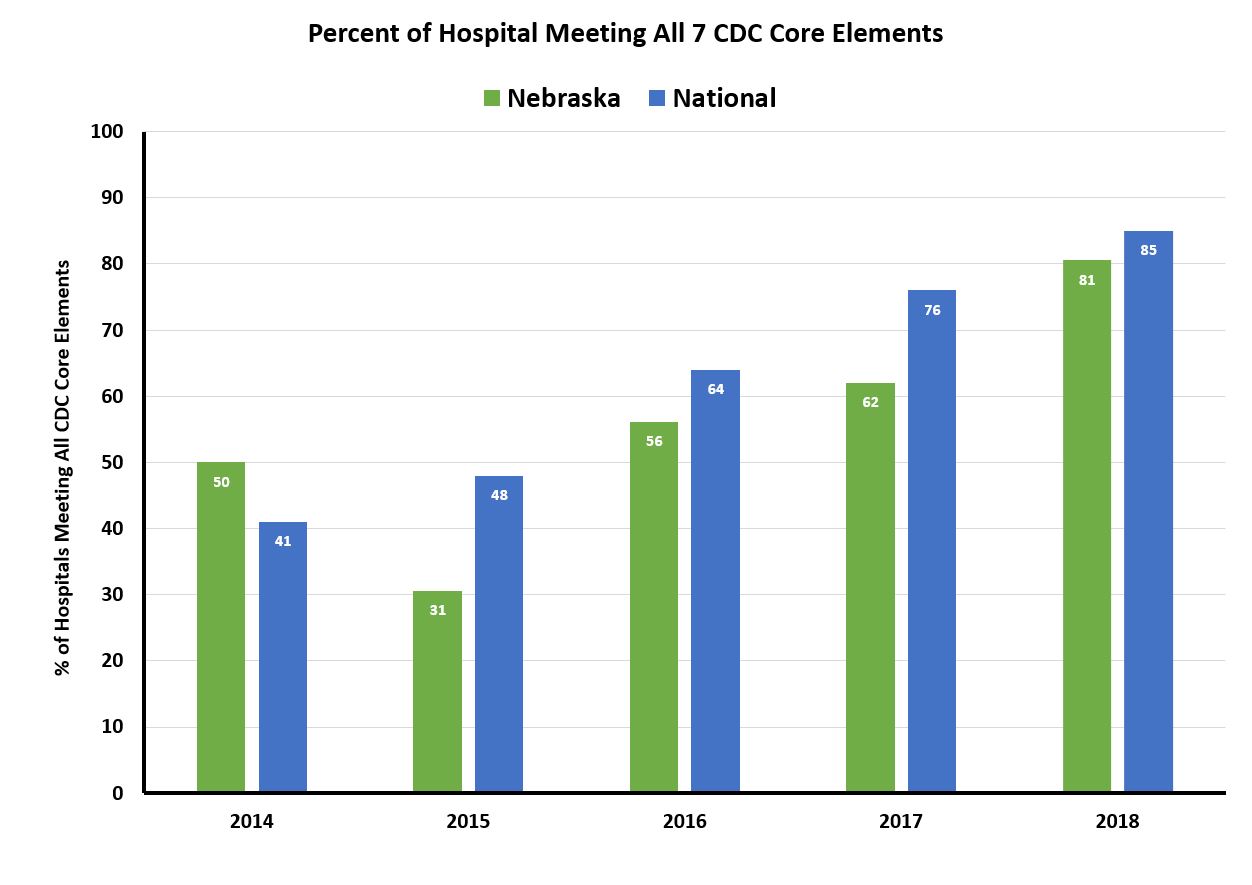
These efforts have produced positive outcomes in the implementation of antimicrobial stewardship programs and antimicrobial use in the outpatient settings nationally and in Nebraska. Since the publication of the CDC Core Elements for Hospital Antibiotic Stewardship Program in 2014, the number of hospitals implementing all 7 core elements of antimicrobial stewardship program have increased both nationally and in Nebraska.
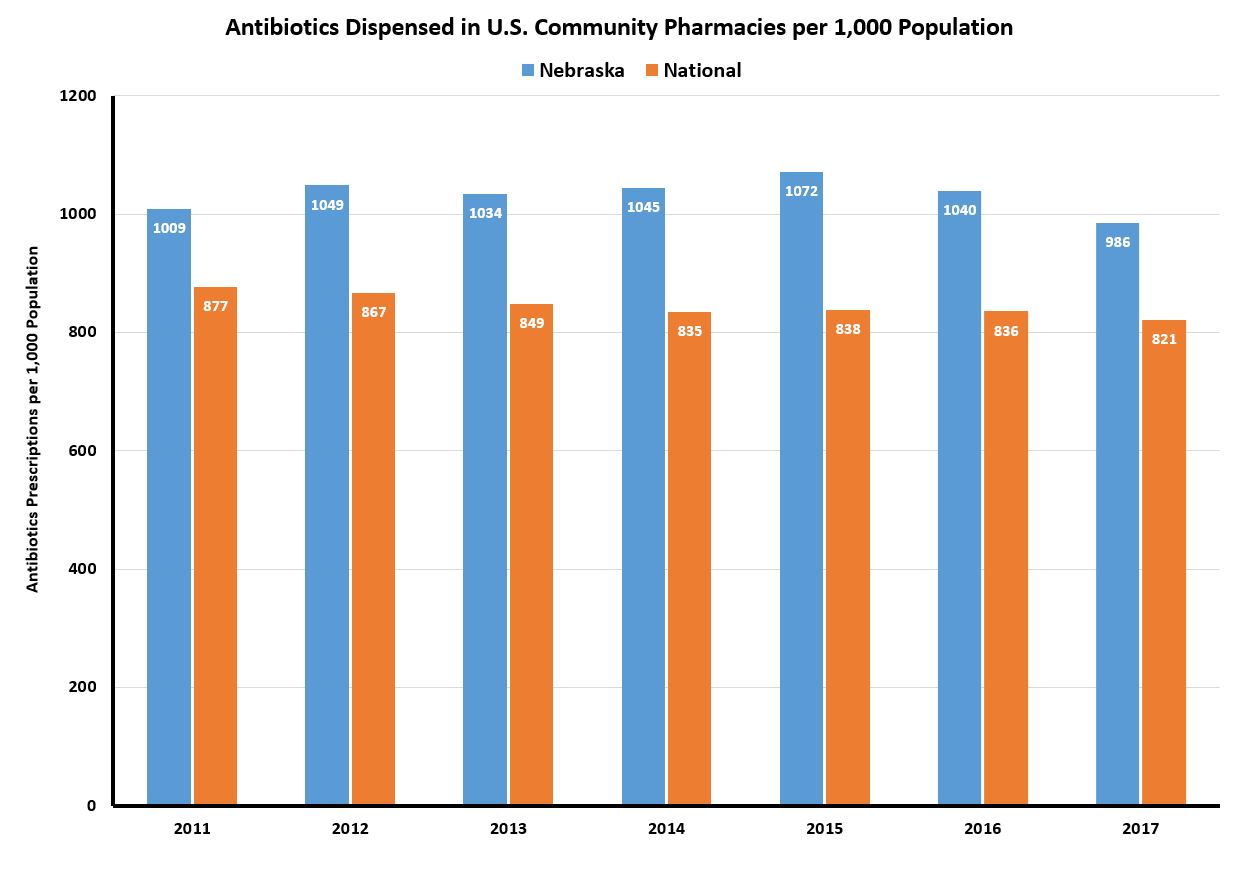
 Another area where positive impact has been realized with the emphasis on antimicrobial stewardship is outpatient antibiotic prescribing. Nationally, the rates of outpatient antibiotic prescriptions have been steadily decreasing between 2011 to 2017. However, a consistent trend in reduction of outpatient antibiotic prescribing during this period was less apparent in Nebraska until more recently. The 2017 outpatient antibiotic prescribing rate of 986 prescriptions per 1,000 population signified the second consecutive year of decline and the first time prescribing rate fell below 1,000.
Another area where positive impact has been realized with the emphasis on antimicrobial stewardship is outpatient antibiotic prescribing. Nationally, the rates of outpatient antibiotic prescriptions have been steadily decreasing between 2011 to 2017. However, a consistent trend in reduction of outpatient antibiotic prescribing during this period was less apparent in Nebraska until more recently. The 2017 outpatient antibiotic prescribing rate of 986 prescriptions per 1,000 population signified the second consecutive year of decline and the first time prescribing rate fell below 1,000.
Despite the encouraging data on these and other infection-related parameters in Nebraska (see Dr. Salman Ashraf’s UNMC ID blog), room for improvement exists. In recognition of Antibiotic Awareness Week, the Nebraska Department of Health and Human Services (DHHS) released a health alert update outlining 6 strategies in the areas of detection, containment and prevention to reduce the threats of antimicrobial resistance in Nebraska.
Detection:
–Use the state-of-the-art antimicrobial susceptibility data mart which captures data from >90% of laboratories in Nebraska to detect and tract resistant organisms such as carbapenem-resistant Enterobacteriaceae (CRE)
Containment:
–Reduce transmission of highly antimicrobial resistant organisms through appropriate contact precaution/isolation, colonization testing of potentially exposed patients, and communication at the time of patient transfer between different healthcare facilities
Preventions (4 strategies):
–Promote vaccination against influenza and Streptococcus pneumoniae to reduce post-influenza bacterial pneumonia and invasive pneumococcal disease, respectively
–Improve infection prevention practices to prevent transmission of multidrug resistant organisms
–Implement appropriate diagnostic stewardship to test for infections only in symptomatic patients
–Improve antimicrobial use and prescribing by implementing antimicrobial stewardship in all levels of healthcare
Healthcare facilities are encouraged to adopt these strategies to maintain the comparative low and reverse the rising rate of carbapenemase-producing CRE (CP-CRE) in Nebraska.