Syphilis

- STIs including syphilis are increasing across the US, including Nebraska!
- Use our ASAP resources to:
- Review appropriate syphilis treatment
- Manage the nationwide injectable penicillin shortage
- Better manage a patient with a history of reported penicillin allergy
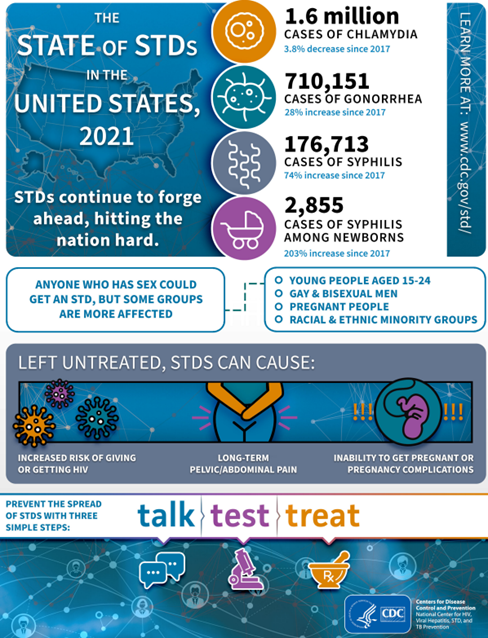
Image source: TheStateOfSTDs.psd (cdc.gov)
Section I: Syphilis Treatment
Treatment
Penicillin G, administered parenterally, is the preferred drug for treating patients in all stages of syphilis. The preparation used (i.e., benzathine, aqueous procaine, or aqueous crystalline), dosage, and length of treatment depend on the stage and clinical manifestations of the disease. Treatment for late latent syphilis (>1 years’ duration) and tertiary syphilis requires a longer duration of therapy. Longer treatment duration is required for persons with latent syphilis of unknown duration to ensure that those who did not acquire syphilis within the preceding year are adequately treated.
Primary, Secondary, or Early Latent (<1 year)
Benzathine penicillin G 2.4 million units IM in a single dose
Late Latent (>1 year), Latent Syphilis of Unknown Duration, or Tertiary Syphilis with Normal CSF Examination
Benzathine penicillin G 7.2 million units total, administered as 3 doses of 2.4 million units IM each at 1-week intervals
Neurosyphilis, Ocular Syphilis
Aqueous crystalline penicillin G 18-24 million units per day, administered as 3-4 million units IV every 4 hours or continuous infusion, for 10-14 days
- Additional doses of benzathine penicillin are not indicated in patients with HIV infection
- Additional doses of penicillin in pregnant women with early syphilis may be indicated if evidence of fetal syphilis on ultrasound
Selection of the appropriate penicillin preparation is important because T. pallidum can reside in sequestered sites (e.g., the CNS and aqueous humor) that are poorly accessed by certain forms of penicillin. Combinations of benzathine penicillin, procaine penicillin, and oral penicillin preparations are not considered appropriate for syphilis treatment. Reports have indicated that practitioners have inadvertently prescribed combination long- and short-acting benzathine-procaine penicillin (Bicillin C-R) instead of the standard benzathine penicillin product (Bicillin L-A) recommended in the United States for treating primary, secondary, and latent syphilis. Practitioners, pharmacists, and purchasing agents should be aware of the similar names of these two products to avoid using the incorrect combination therapy agent for treating syphilis.
Penicillin’s effectiveness for treating syphilis was well established through clinical experience even before the value of randomized controlled clinical trials was recognized. Therefore, approximately all recommendations for treating syphilis are based not only on clinical trials and observational studies, but on many decades of clinical experience.
Special Considerations
Pregnancy
Parenteral penicillin G is the only therapy with documented efficacy for syphilis during pregnancy. Pregnant women with syphilis at any stage who report penicillin allergy should be desensitized and treated with penicillin (see section on Managing Patients with a History of Penicillin Allergy).
Jarisch-Herxheimer Reaction
The Jarisch-Herxheimer reaction is an acute febrile reaction frequently accompanied by headache, myalgia, and fever that can occur within the first 24 hours after the initiation of any syphilis therapy; it is a reaction to treatment and not an allergic reaction to penicillin. Patients should be informed about this possible adverse reaction and how to manage it if it occurs. The Jarisch-Herxheimer reaction occurs most frequently among persons who have early syphilis, presumably because bacterial loads are higher during these stages. Antipyretics (such as acetaminophen) can be used to manage symptoms; however, they have not been proven to prevent this reaction. The Jarisch-Herxheimer reaction might induce early labor or cause fetal distress in pregnant women; however, this should not prevent or delay therapy.
Management of Sex Partners
Sexual transmission of T. pallidum is thought to occur only when mucocutaneous syphilitic lesions are present. Such manifestations are uncommon after the first year of infection. Persons exposed through sexual contact with a person who has primary, secondary, or early latent syphilis should be evaluated clinically and serologically and treated according to CDC recommendations Syphilis – STI Treatment Guidelines (cdc.gov)
Doxycycline Post-Exposure Prophylaxis
What is doxy-PEP?
Post-exposure prophylaxis (PEP) is a treatment given after a potential exposure to a disease to try to prevent the disease from occurring. Emerging evidence from a study among men who have sex with men (MSM) and transgender women (TGW) suggests that doxycycline taken soon after condomless oral, anal, or vaginal sex, significantly reduces acquisition of chlamydia (CT), gonorrhea (GC), and syphilis.1 Doxycycline is used as a first line treatment for chlamydia, a second line treatment for syphilis, and additionally has some efficacy against gonorrhea, making it an appealing option for use as PEP (known as doxy-PEP).
Which patients could be considered for doxy-PEP and how should it be prescribed?
- Consider providing doxy-PEP to men who have sex with men (MSM) or transgender women (TGW) who have had ≥1 bacterial STI in the past 12 months.
- Prescribe 200 mg of doxycycline to be taken ideally within 24 hours (no later than 72 hours) after condomless oral, anogenital, or vaginal sex. Doxycycline can be taken daily depending on sexual activity, but no more than 200 mg every 24 hours.
- Doxycycline hyclate or monohydrate immediate release 100 mg (2 tabs taken simultaneously)
- Immediate release is typically less expensive than delayed release. Doxycycline hyclate delayed release 200 mg (1 tab) while more expensive may have fewer gastrointestinal side effects.
- It is recommended that 30 treatment courses be provided (30-60 tablets depending on doxycycline formulation) with 1-2 refills with follow-up required in 3 months. There is no routine monitoring of the doxycycline therapy required.
- Doxycycline hyclate or monohydrate immediate release 100 mg (2 tabs taken simultaneously)
- If needed for clinic visit coding: ICD10 diagnosis code: Z20.2 (Contact with and (suspected) exposure to infections with a predominantly sexual mode of transmission)
- Prescribe 200 mg of doxycycline to be taken ideally within 24 hours (no later than 72 hours) after condomless oral, anogenital, or vaginal sex. Doxycycline can be taken daily depending on sexual activity, but no more than 200 mg every 24 hours.
- Provide comprehensive preventative sexual health counseling and education to all sexually active individuals including HIV/STI screening, doxy-PEP, HIV pre-exposure prophylaxis CDC HIV PrEP Guidelines, HIV post-exposure prophylaxis CDC PEP Guidelines, vaccinations (e.g. Hepatitis A/B, Human Papilloma Virus (HPV), Meningococcal, expedited partner therapy (Legal Status of EPT – Nebraska (cdc.gov)), and/or contraception where warranted.
- Pre-prescription screening: At initiation of doxy-PEP and every three months, screen for GC and CT at all anatomic sites of exposure (urogenital, pharyngeal, and/or rectal), as well as testing for syphilis and HIV (if not known PLWH). If diagnosed with an STI, patients should be treated according to CDC STI Treatment Guidelines.
How should patients receiving doxy-PEP prescriptions be counseled?
How well does this strategy work for STI prevention?
- In one study, doxy-PEP reduced syphilis by 77-87%, chlamydia by 74-88% and gonorrhea by 55-57%.1
- Since doxy-PEP is not 100% effective in preventing STIs, routine testing for STIs should continue as per CDC recommendations including quarterly testing for chlamydia, gonorrhea, and syphilis.
- Doxy-PEP does not prevent viral infections (HIV, Mpox, HPV or HSV).
- Patients should be counseled on safe sex practices to prevent sexually transmitted diseases. Prevention – STD Information from CDC
When should doxy-PEP be taken?
- 200 mg of doxycycline should be taken within 24 hours and no later than 72 hours after condomless oral, anal or vaginal sex. Doxycycline can be taken as often as every day, depending on frequency of sexual activity, but individuals should not take more than 200 mg within a 24-hour period.
What are important safety considerations?
- People taking doxycycline should be counseled about possible drug interactions, risk of sun sensitivity, gastrointestinal symptoms, remaining upright for 30 minutes after taking doxycycline to reduce the risk of pill esophagitis, and the rare risk of benign intracranial hypertension and other serious side effects – doxycycline FDA label.
- Doxycycline is generally safe and well tolerated. Long-term use of doxycycline has been prescribed safely for many years for other medical indications such as acne treatment and malaria.
- Doxycycline should not be taken during pregnancy due to the knowledge that tetracyclines cause cosmetic staining of the primary dentition in fetuses exposed during the second or third trimester of pregnancy and manufacturer concerns about possible enamel hypoplasia and depression of fetal bone growth. Doxy-PEP use should be avoided in women of childbearing age.
What are some other considerations for prescribers and pharmacists to keep in mind?
Should we be worried about causing further bacterial resistance by using doxy-PEP?
As this is a novel strategy, no data exists on the likelihood of creating antimicrobial resistance. Any use of antibiotics may lead to resistance. Data are being collected and reviewed for possible antimicrobial resistance among bacterial STIs (gonorrhea and chlamydia), commensal Neisseria (potential reservoir for tetracycline resistant plasmids), and community-acquired Staphylococcus aureus.
What effect will doxy-PEP have on the gut microbiome?
Study data on the impact of doxy-PEP on the gut microbiome are being collected and reviewed. All antibiotics carry a risk of causing Clostridioides difficile (C. diff) infection, but antibiotics such as doxycycline have a much lower risk than other antibiotic classes.
Can doxy-PEP be used in other patient populations?
In a recent randomized trial of 449 cisgender Kenyan women, doxy-PEP was not shown to be protective against STIs.2 Right now, the evidence supports use of PEP in gay and bisexual MSM and transgender women. There is significant pause on prescribing this for cisgender, heterosexual women because of the study from Kenya. More data are needed to better understand the reasons why doxy-PEP was found to be ineffective among women in the Kenya study, including assessments of adherence.
Does the CDC have recommendations for use of doxy-PEP?
- Use of doxy-PEP as a strategy to reduce sexually transmitted infections is still in its early days. Doxycycline is not FDA approved for STI PEP and there is no national organizational guidance for its use as STI prevention. However, the CDC has released considerations for doxy-PEP as an STI preventative strategy and further guidance for clinicians will likely be available soon.
- Other state jurisdictions have already begun to employ doxy-PEP as a strategy to combat rising rates of STIs
References and Additional Resources:
- Luetkemeyer et al. Postexposure Doxycycline to Prevent Bacterial Sexually Transmitted Infections N Engl J Med. 2023;388(14):1296-1306. doi:10.1056/NEJMoa2211934
- Stewart et al. “Doxycycline Postexposure Prophylaxis for Prevention of STIs among Cisgender Women.” Oral Abstract 121 at: Conference on Retroviruses and Opportunistic Infections (CROI); 2023 Feb 19-22; Seattle, Washington.
- Nebraska:
- CDC:
- California Prevention Training Center – Educational opportunities and training materials
Additional Resources
Section II: Penicillin Drug Shortage
Temporary Importation of Benzathine Penicillin to Address Supply Shortage
Bicillin L-A® Shortage
The FDA has listed penicillin G benzathine injectable suspension on their Drug Shortages webpage, noting limited supply due to increased demand.
Bicillin L-A® is the first-line recommended treatment for syphilis and the only recommended treatment option for some patients.
During the shortage, clinics and hospitals should:
- Continue to follow CDC’s treatment recommendations. Penicillin G benzathine (Bicillin L-A®) is the only recommended treatment for pregnant people infected with or exposed to syphilis.
- Doxycycline 100mg PO BID for two weeks (for early syphilis) or for four weeks (for late latent or syphilis of unknown duration) is an alternative for the treatment of non-pregnant people with a penicillin allergy.
- Prioritize the use of Bicillin L-A® to treat pregnant people and babies with congenital syphilis.
- Avoid use of Bicillin L-A® for treatment of infections other than syphilis (i.e. pharyngitis, skin and soft tissue infections)
- To help CDC continue to monitor the situation, notify DSTDP (stdshortages@cdc.gov) of:
- Shortages or stock-outs of Bicillin L-A® in the jurisdiction.
- Situations in which patients diagnosed with syphilis are not being treated due to the inability to procure Bicillin L-A® in the jurisdiction.
- Report any shortages to the Pfizer Supply Continuity Team at 844-646-4398 (select 1 and then select 3).
Section III: Managing Patients with a History of Penicillin Allergy
Treatment Guidelines
Penicillin is recommended for all clinical stages of syphilis, and no proven alternatives exist for treating neurosyphilis, congenital syphilis, or syphilis during pregnancy.
Penicillin allergy is one of the most frequently reported antibiotic allergies. It is often overreported, and the majority of patients who report penicillin allergy are able to tolerate the medication. Patients often are incorrectly labeled as allergic to penicillin and are therefore denied the benefit of a ß-lactam therapy. The presence of a penicillin allergy label considerably reduces prescribing options for affected patients. Moreover, penicillin allergy labels lead to the use of more expensive and less effective drugs and can result in adverse consequences, including longer length of hospital stay and increased risk for infection.
The overreported prevalence of penicillin allergy is secondary to imprecise use of the term “allergy” by families and clinicians and lack of clarity to differentiate between immunoglobulin E (IgE)-mediated hypersensitivity reactions, drug intolerances, and other idiosyncratic reactions that can occur days after exposure. Approximately 80% of patients with a true IgE-mediated allergic reaction to penicillin have lost the sensitivity after 10 years. Thus, patients with recent reactions are more likely to be allergic than patients with remote reactions, and patients who had allergic reactions in the distant past might no longer be reactive.
In a Baltimore, Maryland, STI clinic study, only 7.1% of the patients who reported allergy to penicillin or to another ß-lactam antibiotic had an objective positive test for penicillin allergy. Moreover, in studies that have incorporated penicillin skin testing and graded oral challenge among persons with reported penicillin allergy, the true rates of allergy are low, ranging from 1.5% to 6.1%.2-4 In hospitalized patients and other populations with comorbidities, the typical rates of validated penicillin allergy among patients who report a history of penicillin allergy are 2.5%–9.0%.6-8
Patients at Low Risk for Oral Challenge
If the patient gives only a low-risk history of IgE-mediated penicillin allergy that includes symptoms such as those listed below, an oral challenge (oral one-time dose of amoxicillin 250 mg) can be administered to document the absence of allergy. If the reaction occurred in the distant past (>10 years), the likelihood is reduced even further. The risk for severe amoxicillin-mediated anaphylaxis has decreased over time and is rare.
Low risk history in patients who report Penicillin allergy (Give Oral Challenge)
- Gastrointestinal Symptoms
- Headache
- Pruritis without rash
- Localized rash
- Delayed onset rash (>24 hours)
- Symptoms unknown
- Family history of penicillin or other drug allergy
- Patient denies allergy, but it is on the medical record
Similar to in-clinic vaccine administration, clinics planning to administer an oral amoxicillin challenge to low-risk patients should have a plan in place to manage potential reactions. Rescue medications including oral diphenhydramine and IM epinephrine should be readily accessible and clinic staff should be provided with education on reaction management steps. The clinic plan should include processes for transferring the patient to a higher level of care in the event of anaphylaxis (i.e. emergency department).
Reactions during oral amoxicillin challenge in low-risk patients are uncommon. In one study conducted in a primary care clinic, 3% of patients (3/99) receiving an oral amoxicillin challenge had minor cutaneous reactions (i.e. itching) and were treated with oral diphenhydramine (none received epinephrine).4
Monitoring the patient in the clinic for 60 minutes after ingestion of the oral amoxicillin challenge is recommended. Patients should be observed for life-threatening immediate reactions including hypotension and bronchospasm.9
Skin Testing for Penicillin Allergy
Skin testing for penicillin allergy should be performed if any indication exists that the symptoms were secondary to an IgE-mediated hypersensitivity. Testing is also indicated as a potential diagnostic procedure to definitively rule out penicillin allergy and document a negative allergy status in the medical record (i.e., delabeling). Penicillin skin testing has become a clinically significant element in antibiotic stewardship programs, and the procedure has been increasingly used by hospital-based pharmacists, hospitalists, and infectious disease physicians as part of overall antibiotic stewardship interventions. When integrated into stewardship, the rates of ß-lactam antibiotic use increased substantially.
Persons with negative results of a penicillin skin test, followed by an amoxicillin oral challenge, can receive conventional penicillin therapy safely if needed. Persons with positive skin test results and for whom no other clinical options exist (e.g., neurosyphilis and syphilis in a pregnant woman) should be referred to an allergist and desensitized before initiating treatment.
Desensitization
Desensitization is required for persons who have a documented penicillin allergy and for whom no therapeutic alternatives exist (e.g., syphilis during pregnancy and persons with neurosyphilis). Modified protocols might be considered on the basis of the clinical syndrome, drug of choice, and route of administration. Patients might require referral to a specialty center where desensitization can be performed.
References
- Gadde J, Spence M, Wheeler B, Adkinson NF Jr. Clinical experience with penicillin skin testing in a large inner-city STD clinic. JAMA 1993;270:2456–63
- Tucker MH, Lomas CM, Ramchandar N, Waldram JD. Amoxicillin challenge without penicillin skin testing in evaluation of penicillin allergy in a cohort of Marine recruits. J Allergy Clin Immunol Pract 2017;5:813–5
- Goldberg A, Confino-Cohen R. Skin testing and oral penicillin challenge in patients with a history of remote penicillin allergy. Ann Allergy Asthma Immunol 2008;100:37–43.
- Iammatteo M, Alvarez Arango S, Ferastraoaru D, et al. Safety and outcomes of oral graded challenges to amoxicillin without prior skin testing. J Allergy Clin Immunol Pract 2019;7:236–43.
- Trubiano JA, Thursky KA, Stewardson AJ, et al. Impact of an integrated antibiotic allergy testing program on antimicrobial stewardship: a multicenter Clin Infect Dis 2017;65:166–74.
- Siew LQC, Li PH, Watts TJ, et al. Identifying low-risk beta-lactam allergy patients in a UK tertiary centre. J Allergy Clin Immunol Pract 2019;7:2173–e1.
- Chen JR, Tarver SA, Alvarez KS, Tran T, Khan DA. A proactive approach to penicillin allergy testing in hospitalized patients. J Allergy Clin Immunol Pract 2017;5:686–93
- Leis JA, Palmay L, Ho G, et al. Point-of-care β-lactam allergy skin testing by antimicrobial stewardship programs: a pragmatic multicenter prospective evaluation. Clin Infect Dis 2017;65:1059–65.
- Gateman DP, Rumble JE, Protudjer JLP, Kim H. Amoxicillin oral provocation challenge in a primary care clinic: a descriptive analysis. CMAJ Open. 2021 Apr 16;9(2):E394-E399.
Additional Resources
Request for Information
Names of clinics in various local health department jurisdictions that are accepting referrals for evaluation of patients suspected of having syphilis and also have IM Benzathine Penicillin G injections available for treatment, if needed.
Douglas County Health Department (DCHD)
Clinic Name: UNMC Infectious Diseases Clinic
Clinic Address/Location: 4400 Emile Street, Omaha, NE 68198 (On 5th floor of Durham Outpatient Center)
Best way for a provider to refer a patient to the clinic: (402) 559-4015
Clinic Name: Charles Drew Health Center
Clinic Address/Location: 2915 Grant Street, Omaha, NE 68111
Best way for a provider to refer a patient to the clinic: (402) 451-3553 (Phone) or (402) 453-2061 (Fax)
Clinic Name: Douglas County Health Department
Clinic Address/Location: 1111 South 41st Street, Suite 210, Omaha, NE 68105
Best way for a provider to refer a patient to the clinic: (402) 444-7112
Clinic Name: OthroNebraska Emergency Department (not a clinic)
Clinic Address/Location: 2727 S. 144th Street, Suite 150, Omaha, NE 68144
Best way for a provider to refer a patient to the clinic: (402) 609-3333 or email chris.vollmuth@orthonebraska.com
Elkhorn Logan Valley Public Health Department (ELVPHD)
Clinic Name: Midtown Health Center – Norfolk
Clinic Address/Location: 302 West Phillip Ave, Norfolk, NE 68701
Best way for a provider to refer a patient to the clinic: (402) 371-8000 (Phone) or (402) 371-0971 (Fax)
Clinic Name: Midtown Health Center – Madison
Clinic Address/Location: 222 Main Street, Madison, NE 68748
Best way for a provider to refer a patient to the clinic: (402) 371-8000 (Phone) or (402) 371-0971 (Fax)
Clinic Name: Midtown Health Center – West Point
Clinic Address/Location: 303 Plaza Drive, West Point, NE 68788
Best way for a provider to refer a patient to the clinic: (402) 371-8000 (Phone) or (402) 371-0971 (Fax)
Four Corners Health Department (FCHD)
Clinic Name: York General Hospital
Clinic Address/Location: 2222 North Lincoln Ave, York, NE 68843
Best way for a provider to refer a patient to the clinic: (402) 362-6671
Clinic Name: Henderson Health Care
Clinic Address/Location: 1621 Front Street, Henderson, NE 68371
Best way for a provider to refer a patient to the clinic: (402) 723-4512
Clinic Name: Butler County Health Care Center
Clinic Address/Location: 372 South 9th Street, David City, NE 68632
Best way for a provider to refer a patient to the clinic: (402) 367-1219
Clinic Name: Seward Family Medical Clinic
Clinic Address/Location: 250 North Columbia Avenue, Seward, NE 68434
Best way for a provider to refer a patient to the clinic: (402) 643-4800
Clinic Name: Utica Family Medical Center
Clinic Address/Location: 100 4th Street, Utica, NE 68456
Best way for a provider to refer a patient to the clinic: (402) 534-2081
Clinic Name: Milford Family Medical Center
Clinic Address/Location: 119 South C Street, Milford, NE 68405
Best way for a provider to refer a patient to the clinic: (402) 761-3307
Lincoln-Lancaster County Health Department (LLCHD)
TEMPORARILY OUT OF PENICILLIN
Clinic Name: Lincoln-Lancaster County Health Department
Clinic Address/Location: 3131 O street, Lincoln, NE 68510
Best way for a provider to refer a patient to the clinic: (402) 441-8054
Clinic Name: Family Health Services – Lincoln
Clinic Address/Location: 5000 St Paul Ave, Burt Hall North Lincoln, NE 68504
Best way for a provider to refer a patient to the clinic: (402) 466-1012
Clinic Name: Planned Parenthood – Lincoln Health Center
Clinic Address/Location: 5631 S 48th St #100, Lincoln, NE 68516
Best way for a provider to refer a patient to the clinic: (877) 859-0587
Loup Basin Public Health Department (LBPHD)
Clinic Name: Valley County Health System
Clinic Address/Location: 2701 L St. Ord, NE 68862
Best way for a provider to refer a patient to the clinic: (308) 728-4312
Northeast Nebraska Public Health Department (NNPHD)
Clinic Name: Pender Medical Clinic
Clinic Address/Location: 958 Wellness Way, Pender, NE 68047
Best way for a provider to refer a patient to the clinic: (402) 385-1963
North Central District Health Department (NCDHD)
Clinic Name: Antelope Memorial Hospital
Clinic Address/Location: 102 W 9th Street, Neligh, Nebraska 68756
Best way for a provider to refer a patient to the clinic: (402) 887-6379
Clinic Name: Antelope Memorial Hospital, Neligh Clinic
Clinic Address/Location: 109 West 1th Street, Neligh, Nebraska 68756
Best way for a provider to refer a patient to the clinic: (402) 887-6311
Clinic Name: Cherry County Hospital
Clinic Address/Location: 510 North Green Street, Valentine, Nebraska 69201
Best way for a provider to refer a patient to the clinic: (402) 376-2525
Clinic Name: Cherry County Clinic
Clinic Address/Location: 512 North Green Street, Valentine, Nebraska 69201
Best way for a provider to refer a patient to the clinic: (402) 376-3770
Clinic Name: Avera Medical Group Crofton
Clinic Address/Location: 203 West Main Street, Crofton, Nebraska 68730
Best way for a provider to refer a patient to the clinic: (402) 388-2343
Clinic Name: Avera Medical Group O’Neill
Clinic Address/Location: 300 North 2nd Street, Suite 100, O’Neill, Nebraska 68763
Best way for a provider to refer a patient to the clinic: (402) 336-2900
Clinic Name: Greater Sandhills Atkinson
Clinic Address/Location: 418 East 5th Street, Atkinson, Nebraska 68713
Best way for a provider to refer a patient to the clinic: (402) 925-2994
Clinic Name: Greater Sandhills Bassett
Clinic Address/Location: 101 East South Street, Bassett, Nebraska 68714
Best way for a provider to refer a patient to the clinic: (402) 684-2285
Clinic Name: Greater Sandhills Stuart
Clinic Address/Location: PO Box 70, Stuart, Nebraska 68780
Best way for a provider to refer a patient to the clinic: (402) 924-3777
Clinic Name: West Holt Hospital
Clinic Address/Location: 406 West Neely Street, Atkinson, Nebraska 68713
Best way for a provider to refer a patient to the clinic: (402) 925-2811
Clinic Name: West Holt Medical Clinic
Clinic Address/Location: 405 West Pearl Street, Atkinson, Nebraska 68713
Best way for a provider to refer a patient to the clinic: (402) 925-2811
Clinic Name: Santee Health Center
Clinic Address/Location: 110 Visiting Eagle Street, Verdel, Nebraska 68760
Best way for a provider to refer a patient to the clinic: (402) 857-2300
Panhandle Public Health District (PPHD)
Clinic Name: Sidney Regional Medical Center
Clinic Address/Location: 1000 Pole Creek Crossing, Sidney, NE 69162
Best way for a provider to refer a patient to the clinic: (308) 254-5544 (Phone); (308) 254-2672 (Fax)
Clinic Name: Alliance Children’s and Allied Health
Clinic Address/Location: 204 E 3rd Street, Alliance, NE 69301
Best way for a provider to refer a patient to the clinic: (308) 761-1151
Clinic Name: Community Action Health Center
Clinic Address/Location: 975 Crescent Dr, Gering, NE 69341
Best way for a provider to refer a patient to the clinic: (308) 633-2770
Scotts Bluff County Health Department (SBCHD)
Clinic Name: RWPC Family Medicine
Clinic Address/Location: 3911 Avenue B, Suite 1100, Scottsbluff, NE 69361
Best way for a provider to refer a patient to the clinic: (308) 630-2100 (Phone) or (308) 630-2149 (Fax)
South Heartland District Health Department (SHDHD)
Clinic Name: Hastings Family Care
Clinic Address/Location: 223 East 14th Street, Suite 100, Hastings, NE 68901
Best way for a provider to refer a patient to the clinic: (308) 632-2540
Southwest Nebraska Public Health Department (SNPHD)
Clinic Name: Chase County Clinic
Clinic Address/Location: 600 West 12th Street, Imperial, NE 69033
Best way for a provider to refer a patient to the clinic: (308) 882-7225
Two Rivers Public Health Department (TRPHD)
Clinic Name: Children’s Physicians
Clinic Address/Location: 211 West 33rd Street, Kearney, Nebraska 68845
Best way for a provider to refer a patient to the clinic: (308) 234-5613
West Central District Health Department (WCDHD)
Clinic Name: Great Plains Family Medicine (via Great Plains Infectious Disease referral)
Clinic Address/Location: 500 West Leota St. Suite 100, North Platte, NE 69101
Best way for a provider to refer a patient to the clinic: (308) 568-4700
Clinic Name: Great Plains Health Infectious Diseases
Clinic Address/Location: 611 West Francis St. Suite 200, North Platte, NE 69101
Best way for a provider to refer a patient to the clinic: (308) 568-3500 (Phone) or (308) 568-3578 (Fax)



