Addressing Reported Penicillin Allergy – A 2022 Practice Parameter Update

Addressing Reported Penicillin Allergy – A 2022 Practice Parameter Update
Antibiotic Awareness Week 2022
Patient reported antibiotic allergies present clinicians with challenging decisions at the point of prescribing. Approximately half of all patients admitted to the hospital receive antibiotics, and 25% of inpatients who require antibiotics report at least one antimicrobial drug allergy.1 Specifically, penicillin (PCN) allergy is reported in up to 10% of the general population and up to 16% of inpatients.1-3
Patients with reported PCN allergies often receive more costly and broad-spectrum antibiotics than patients without these reported allergies.1 Furthermore, many patients with reported PCN allergy are not receiving drugs, such as later-generation cephalosporins and carbapenems, that are safely tolerated despite a PCN allergy.1,4
If you find that deciding which antibiotics can be safely prescribed in the setting of a patient reported penicillin allergy is challenging, you are not alone! A survey of 521 providers at Mass General highlighted that 42% of providers reported no prior education in antibiotic drug allergies, and only 68% reported feeling prepared to prescribe antibiotics for the penicillin-allergic patient.6 In fact, in the survey responses only 37% would prescribe ceftriaxone, 46% would prescribe cefepime, and 66% would prescribe meropenem, even though all of these agents are safe in most penicillin-allergic patients.6
Strategies for Penicillin Allergy De-labeling
Reported allergies to PCN, however, do not equate with true IgE-mediated allergy. After formal allergy evaluation, including skin testing, up to 99% of patients with reported PCN allergy are found not to be allergic.5 There are multiple strategies for penicillin allergy de-labeling that are primarily based on the history of the reaction and patient comorbidities. These strategies include:
- Medication history
- For patients with histories that are inconsistent with penicillin allergy (such as headache, GI upset, or family history of penicillin allergy), no testing is required, and the patient may be de-labeled7
- In Nebraska, pharmacists have access to the Prescription Drug Monitoring Program (PDMP) database which can be helpful to clarify prescription history
- Oral antibiotic challenge
- For patients with histories that are remote and benign, direct oral antibiotic challenge without preceding skin testing is the preferred approach7
- In patients who are reluctant to accept the removal of a penicillin allergy after appropriate counseling, oral amoxicillin challenge using a single treatment dose is sufficient to rule out an allergy (and to gain acceptance of the de-labeling).7
- Penicillin skin testing
- While penicillin skin testing has been the most carefully studied skin test reagent for drug allergy, penicillin skin testing is best used primarily for patients with a history of anaphylaxis, or a recent reaction suspected to be IgE-mediated (eg, immediate onset urticaria)7
- For patients who are particularly anxious or uncomfortable with the idea of a direct challenge, performing penicillin skin tests first may be considered, because confirmation of negative penicillin skin testing may be useful to alleviate these fears.
- Graded challenge
- A graded challenge is an administration of progressively increasing doses of a medication until a full dose is reached. The intention is to verify that a patient will not experience an immediate adverse reaction to a drug. A graded challenge typically involves a few doses over a shorter duration and is not intended to induce drug tolerance.
- Desensitization
- The goal of desensitization is induction of temporary immune drug tolerance by which effector cells are rendered less reactive or nonreactive to igE-mediated immune responses by rapid administration of incremental doses. This strategy involves many steps and is time intensive. Desensitization should only be considered when there are no reasonable alternatives. It is important to remember that drug desensitization is temporary and must be repeated if the patient needs treatment again in the future.
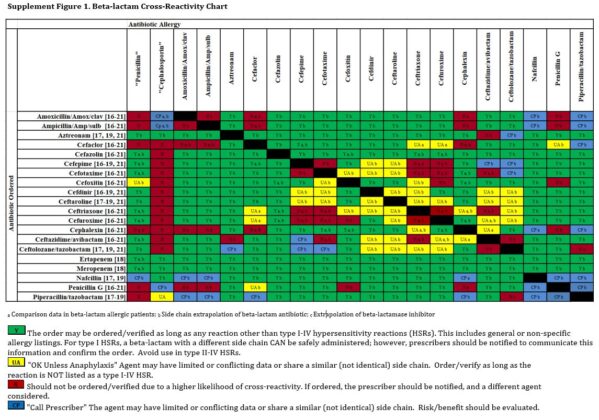
Beta-lactam Cross-Reactivity
Several recent studies indicate that the risk of cross-reactivity among beta-lactams is lower than previous reports suggested.7 Patients with a history of an unverified non-anaphylactic penicillin allergy may have any cephalosporin administered routinely without testing or additional precautions. For example, patients with a history of urticaria to a penicillin can receive any cephalosporin routinely without prior testing. The opposite situation has the same recommendation – for patients with a history of an unverified non-anaphylactic cephalosporin allergy, a penicillin can be administered without testing or additional precautions.7
In contrast, for those rare patients with a history of anaphylaxis to penicillin, a non–cross-reactive cephalosporin (e.g., cefazolin) can be administered routinely without prior testing. Implementation of an antibiotic cross-reactivity chart such as the one pictured below combined with enhanced allergy assessment processes can significantly improve the prescribing of β-lactams in the setting of patient reported penicillin allergy.8
Carbapenem Administration
Guidance on administration of carbapenems to patients with penicillin allergy has also changed since the last Drug Allergy Practice Parameter update. The 2022 Practice Parameter Update now suggests that in patients with a history of penicillin or cephalosporin allergy, a carbapenem may be administered without testing or additional precautions regardless of whether the reaction was anaphylactic.7
Written by Jenna Preusker, Pharm.D., BCPS 
Nebraska ASAP Pharmacy Coordinator
References
- Lee CE, Zembower TR, Fotis MA, Postelnick MJ, Greenberger PA, Peterson LR, et al. The incidence of antimicrobial allergies in hospitalized patients: implication regarding prescribing patterns and emerging bacterial resistance. Arch Intern Med 2000;160:2819-22.
- Rimawi RH, Cook PP, Gooch M, Kabchi B, Ashraf, MS, Rimawi BH, et al. The impact of penicillin skin testing on clinical practice and antimicrobial stewardship. J Hosp Med 2013;8:341-5.
- Sade K, Holtzer I, Levo Y, Kivity S. The economic burden of antibiotic treatment of penicillin-allergic patients in internal medicine wards of a general tertiary care hospital. Clin Exp Allergy 2003;33:501-6.
- Pichichero ME. A review of evidence supporting the American Academy of Pediatrics recommendation for prescribing cephalosporin antibiotics for penicillin-allergic patients. Pediatrics 2005;115:1048-57.
- Macy E, Ngor E. Safely diagnosing clinically significant penicillin allergy using only penicilloyl-poly-lysine. J Allergy Clin Immunol Pract 2013;1:258-63.
- Blumenthal K, et al. Survey of inpatient clinical providers’ antibiotic prescribing knowledge. J Allergy Clin Immunol Pract. 2014; 2(4): 407-413.
- Khan D, Banerji A, Blumenthal K, et al. Drug allergy: A 2022 practice parameter update. J Allergy Clin Immunol 2022; In press.
- Collins C, Scheidel C, Anam K, et al. Impact of an antibiotic side-chain-based cross-reactivity chart combined with enhanced allergy assessment processes for surgical prophylaxis antimicrobials in patients with beta-lactam allergies. Clin Infec Dis 2021;72.



